Common Complications with Jaw Surgery

In the realm of orthodontics, the collaboration between orthodontists and oral surgeons plays a crucial role in transforming the lives of patients with severe dental and facial irregularities. Corrective jaw surgery, also known as orthognathic surgery, stands as a significant milestone in the field, aiming to address misaligned jaws and facial structures that cannot be solely corrected through orthodontic treatment. As experts in orthodontics, we understand the intricacies and challenges that patients may face when opting for corrective jaw surgery. This article delves into the common complications associated with jaw surgery, shedding light on its side effects, preparatory measures, and the transition to a successful recovery.
What Is Corrective Jaw Surgery?
In the realm of orthodontics and oral surgery, the intricacies of corrective jaw surgery, also known as orthognathic surgery, are a cornerstone of our collective expertise. This transformative procedure addresses a spectrum of dentofacial deformities and misalignments that go beyond the scope of conventional orthodontic treatment. The collaboration between orthodontists, maxillofacial surgeons, and other healthcare professionals is pivotal in achieving optimal outcomes for patients in need of corrective jaw surgery.
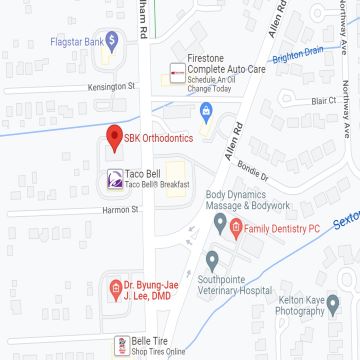
Ann Arbor Orthognathic surgery encompasses a range of procedures designed to reposition the jaws, correct facial asymmetries, and improve overall oral function and aesthetics. This procedure is indicated when severe dental and skeletal discrepancies exist that cannot be solely corrected through orthodontic intervention. Dental malocclusions intertwined with skeletal irregularities often necessitate the expertise of maxillofacial surgeons. Consequentially, common scenarios include mandibular prognathism (an overly prominent lower jaw) and maxillary retrusion (a receded upper jaw), both of which can result in functional impairment, aesthetic concerns, and even temporomandibular joint disorders.
Various surgical techniques are employed to manipulate the jaw bone and achieve the desired corrections. These include sagittal split osteotomy, where the jaw bone is divided and repositioned, and medial osteotomy for upper jaw surgeries. Bimaxillary surgeries involving repositioning of both upper and lower jaws are often conducted to achieve comprehensive results. Moreover, the use of bone plates and screws aids in securing bony segments in their new positions, ensuring stability during healing. Also, distal and proximal segments of the jaws are adjusted to achieve harmony between the upper and lower teeth and improve facial features.
One notable aspect of orthognathic surgery is the consideration of nerve injuries, particularly the alveolar nerve. Thorough preoperative assessment and advanced imaging techniques allow surgeons to minimize the risk of such complications. Surgical advancements, as documented in journals like the Journal of Oral and Maxillofacial Surgery and the International Journal of Oral and Maxillofacial Surgery, have led to refined techniques and improved outcomes, reducing the occurrence of nerve-related issues.
Corrective jaw surgery holds promise in achieving functional and aesthetic improvements and addressing temporomandibular disorders and facial asymmetries. Retrospective studies have shown that the procedure results in enhanced oral function, improved quality of life, and increased self-confidence. For instance, patients with severe mandibular prognathism often benefit from sagittal split advancement osteotomy, which repositions the lower jaw and aligns the mandibular teeth with the upper teeth, thereby improving both occlusion and aesthetics.
Conclusively, corrective jaw surgery is a testament to the synergy between orthodontics and oral surgery. As specialists in the field, we collaborate to deliver comprehensive care, addressing complex dentofacial deformities and improving the lives of patients who require intricate interventions beyond traditional orthodontic approaches.
What Are the Side Effects of Corrective Jaw Surgery?
Undergoing corrective jaw surgery is a significant step towards improved oral function and aesthetics, but like any major surgery, it comes with potential side effects. These can be categorized into short-term complications and long-term effects, each deserving careful consideration.
Short-Term Complications
Short-term complications of corrective jaw surgery may arise immediately after the procedure or during the initial stages of recovery. Research, including retrospective cohort studies and systematic reviews, has shed light on these potential challenges. Postoperative complications might include:
Swelling and Bruising
Swelling and bruising around the surgical sites and face are common after orthognathic surgery. Applying cold compresses and adhering to the recommended postoperative care instructions can help minimize these effects.
Numbness
Numbness in the lower lip, chin, and gums might occur due to nerve manipulation during surgery. Though usually temporary, patients should be informed about the possibility of sensory changes.
Pain and Discomfort
As with any surgical procedure, pain and discomfort are to be expected during the initial stages of recovery. Proper pain management strategies, as prescribed by your surgeon, can alleviate these sensations.
These are common occurrences due to the nature of the surgery. Techniques such as mandibular setback surgery can trigger these reactions due to adjustments in bone positions.
Blood supply and surgical technique play a crucial role in determining the extent of these short-term side effects. The manipulation of bone and tissues during surgery can lead to altered blood flow and potential bruising. However, advancements in surgical techniques, as evidenced by systematic reviews, have contributed to minimizing these issues. Adequate amounts of pain medicine, proper care, and adherence to postoperative instructions can effectively alleviate these initial challenges.
Long-Term Side Effects:
In detailing long-term effects, the focus shifts to factors such as complication rates and potential adjustments required post-surgery. Some patients might require a blood transfusion during or after the procedure due to the extent of the surgery and blood loss. Although relatively uncommon, this consideration underscores the importance of thorough preoperative evaluations.
A pertinent concern in the realm of long-term effects is the need for secondary surgeries to address unforeseen complications or achieve optimal outcomes. These secondary procedures might involve adjustments to bone plates, correction of occlusion, or refinements in aesthetics. Retrospective cohort studies have demonstrated that the likelihood of requiring such secondary interventions varies based on factors such as the complexity of the case, the surgical technique employed, and individual healing responses.
Corrective jaw surgery, while transformative, is not devoid of potential side effects. The distinction between short-term complications and long-term effects serves as a guide for both patients and healthcare professionals alike. With advancements in surgical techniques and a comprehensive approach to preoperative evaluation, the aim is to ensure that the benefits of corrective jaw surgery far outweigh the potential challenges, ultimately leading to enhanced oral function, improved aesthetics, and improved quality of life for the patients in our care.
How to Prepare For Jaw Surgery?
Our collective experience in orthodontics and oral surgery underscores the importance of meticulous preparation for jaw surgery. While general recommendations exist, it’s important to acknowledge that each case demands a unique approach tailored to the patient’s needs and circumstances. So, insights from prospective studies and literature reviews contribute to our comprehensive understanding of the preparatory phase.
General Recommendations
A key aspect of preparing for jaw surgery involves thorough evaluations. Comprehensive dental and medical histories and advanced imaging guide the treatment plan. Orthodontic treatment may be initiated before surgery to align the teeth as closely as possible. Effective communication between the orthodontist, surgeon, and patient is paramount in addressing concerns, setting realistic expectations, and ensuring emotional readiness.
Unique Considerations
Prospective studies have highlighted the importance of addressing specific patient considerations. Patient satisfaction and outcomes are often influenced by factors such as the potential for neuropathic pain or the risk of long-term complications. Understanding these individual nuances informs the preoperative planning process.
While general guidelines provide a foundation, the nuanced understanding of each patient’s unique needs truly drives the preparatory phase. This personalized approach, backed by a wealth of insights from the literature, ensures that patients start their jaw surgery process fully prepared for a successful and transformative outcome.
How to Recover From Orthognathic Surgery?
Our experience in orthodontics and support for oral surgery emphasizes the crucial phase of recovery after orthognathic surgery. Based on clinical practice and research insights, general recommendations guide the recovery process, ensuring patients achieve optimal healing and outcomes.
Immediate Postoperative Care
The initial days after surgery require diligent care. Ice packs applied to the surgical sites help manage swelling, while moist heat can alleviate discomfort in the jaw muscles. Pain after orthognathic surgery is a common concern. Effective interventions for pain, such as prescribed medications, provide relief during this critical period. Patients experiencing pain refractory to standard measures necessitate close monitoring and tailored interventions.
Progressive Recovery
As the weeks and months after surgery unfold, the focus shifts to gradual improvements. Transitioning from a soft diet to regular foods under healthcare professionals’ guidance is essential. Regular follow-up appointments with both the orthodontist and oral surgeon monitor healing progress and provide adjustments for orthodontic appliances if needed. Here is a short list of measures patients must consider for an effective healing transition:
- Follow Postoperative Instructions.
- Pain Management.
- Dietary Adaptations.
- Oral Hygiene.
- Follow-Up Appointments.
- Emotional Support.
Hardware Removal and Neurosensory Alterations
In some cases, plate removal might be necessary after the initial healing period. Patients should expect neurosensory alterations, such as numbness or altered sensations, which often resolve gradually. While hardware removal might alleviate discomfort associated with hardware irritation, these decisions are made on a case-by-case basis.
Recovery from orthognathic surgery requires a structured and informed approach. General recommendations encompassing immediate postoperative care and progressive recovery contribute to successful outcomes. By heeding these insights and collaborating closely with healthcare professionals, patients navigate the recovery phase confidently, achieving optimal healing and restoring oral function.
Unlock Your Perfect Smile with SBK Orthodontics
Having a perfect smile is a process worth a temporary sacrifice. Schedule an appointment at SBK Orthodontics, where our commitment to excellence and your oral health is unparalleled. So, we invite you to experience the difference.
At SBK Orthodontics, our dedicated team of specialists is here to guide kids, teens, and adults alike on the path to a beautiful smile through healthy practices and innovative orthodontic solutions. Our friendly experts are always at your service, ready to address any questions you may have.
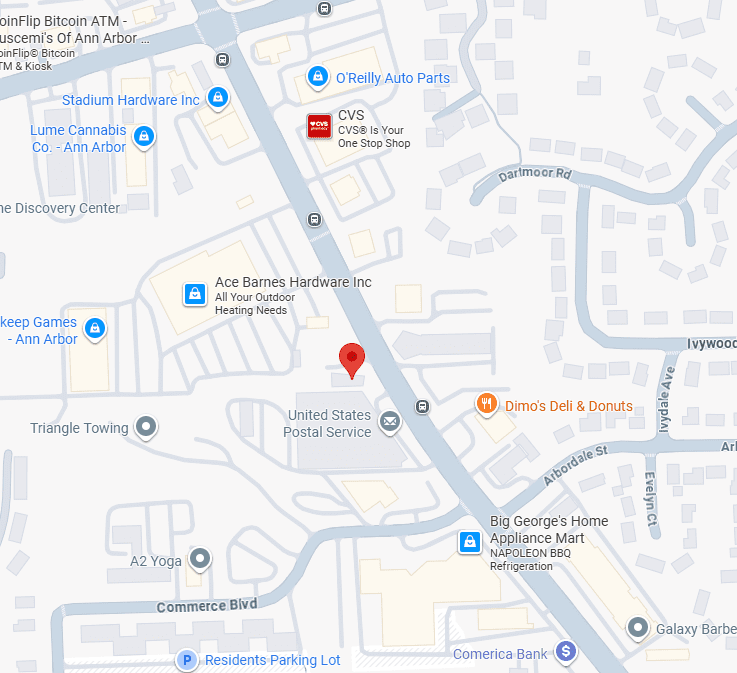
We pride ourselves on delivering high-quality care that goes beyond treatment – it’s about helping you achieve your goals and setting you up for a lifetime of confident, healthy smiles. Our mission resonates in every interaction: to bring top-tier orthodontic practices to Ann Arbor, Taylor, Dexter, Saline, and Chelsea. We’re here to champion oral health in the community and empower you to reach your smile aspirations.
Don’t wait any longer – The moment to have a stunning smile begins here. Schedule your appointment with SBK Orthodontics today and discover the transformation that awaits you.